Contents
NEED OF THE FIRST AID
Prevention is better than cure but when prevention is not possible and an injury does take place, the cure is the only prevention of further injury and this cure is primarily to be provided by First Aid.
First Aid can be defined as an immediate treatment given to the victim of an accident or sudden illness, before -medical help is obtained. It is a combination of simple but quite expedient, active measures to save the victim’s life and prevent possible complications. It needs to be immediate in severe accidents complicated by bleeding, shock, and loss of consciousness.
CLICK HERE FOR 👉 FIRST AID AND NEAR MISS CASE STUDY-1
The majority of accidents are trifle and curable by first aid only. Even otherwise all industrial injuries need immediate first aid for which statutory provisions are also made as follows.
STATUTORY PROVISIONS
Section 45 of the Factories Act requires at least one first aid box or cupboard equipped with the prescribed contents for every 150 workers employed at any one time. It should be readily accessible during all working hours and should be in charge of a qualified person.
For a factory employing more than 500 workers an ambulance room of the prescribed size and contents and in the charge of medical and nursing staff is also required.
Rule 70 of the Gujarat Factories Rules prescribes the contents of a first aid box depending upon the number of persons employed. Rule 70A requires a displayed staling the names and place of availability of the first aider, nearest hospital, and its telephone number.
CLICK HERE FOR 👉 Recognition and Evaluation of Health Hazards
Rule 71 prescribes the. size and other details for an ambulance room or dispensary, a suitable conveyance to remove the victim, and a record of all cases treated. Refer to these rules for the medical items to be kept ready.
Section 41C and Rules 68 R, T, U & V of the Gujarat Factories Rules for Health Records, Medical examinations. Occupational Health Centre, Ambulance Van, etc.
INDIAN STANDARDS
A few IS available for first aid are First aid dressings 11163, pesticide poisoning 4015, radiation protection in medical X-ray equipment of 10 kV to 400 KV 7064, Colour identification of gas cylinders for medical use 3933.
Bandage cotton 863, plaster of Paris IS 4738, 6237, scissors 6252,10384.
CLICK HERE FOR 👉 Measurement of accident
Resuscitators for use with humans IS 13366
GENERAL PRINCIPLES FOR RENDERING FIRST AID
First Aid has five main aims:
- To preserve life.
- To promote or assist recovery.
- To prevent worsening or aggravation of the casualty’s condition.
- To minimize complication and
- To arrange transportation to the hospital if necessary.
First Aid is based on scientific medicine and surgery. It is skilled assistance and makes use of such materials as may be available. But the first aider is not a Doctor. After the doctor takes charge, the first aider’s responsibility ends. He can then stand by to help the doctor.
The first aider should observe carefully, think clearly, and act quickly. He should be calm, cool, and confident. He should not get excited. He should ask someone to call a doctor/inform hospital immediately giving some details of the cases involved. While waiting for the doctor, he should give first aid methodically.
CLICK HERE FOR 👉 WORKPLACE HEALTH AND SAFETY COMMITTEE
Dr. Y. N.Sinha, Dy. Director (Medical) of CLI, Mumbai explains the general meaning of FIRST AID
- First thing first.
- Inform the doctor.
- Reassure the victim.
- Shock prevention or treatment.
- Tourniquet, control bleeding.
- Artificial respiration.
- Immobilize fracture.
- Disposal, send the victim to the hospital.
General Rules of First Aid
The general rules or principles for first aid are as follows:
- Reach the accident spot quickly. This will help to save life.
- Be calm, methodical and quick. By doing so you can lessen the pain and the effects of the injuries which may save a life. Handling the casualty clumsily will only make the final recovery difficult.
- Look for the following: Is there a failure of breathing? Is there severe bleeding? Is the shock light or severe?
CLICK HERE FOR 👉 EMPLOYEES STATE INSURANCE ACT AND RULES
- Attend to these and then treat easily observable injuries.
- Start artificial respiration, if the casualty is not breathing. It must be at once as every second gained is helpful.
- Stop by pressing on the pressure point and press firmly on the bleeding area with a pad and keep up pressing on the bleeding area for at least a few minutes (minimum 3 minutes) by the watch. Take help if needed.
- Treat for shock.
- Avoid handling the casualty unnecessarily.
The priority of Treatment of First Aid treatment
- Examination and Diagnosis.
- Cardio Pulmonary Resuscitation (every second count).
- Control Bleeding.
- Treat Shock and special care of Unconscious cases.
- Fracture (Immobilisation).
- Burn-Cover with clear washed cloth/ dressing and treat shock.
- Eye, Nose and Ear injuries.
- Multiple superficial injuries.
- Transportation and
- Follow up or After-care.
Dr. Subhash Mhaskar (Thane) suggests the following formula for a basic assessment of a serious case:
DR. ABC & Head-Foot Examination :
D = Danger. Please check up first, if there is any sort of danger to the first aider or the patient or to the people around at the ‘spot of the accident in form of poisonous gas, electric current, fire, etc.
R = Response. Call the patient by his name or pinch him and see the response. If no response, the patient is unconscious. Then immediately.
A = Open the Airway by flitting his head to the back and chin up.
B = Check Breathing
C = Check Circulation of blood by checking neck pulse. If the patient is not breathing but the neck pulse is present, give mouth-to-mouth breathing only. If neck pulse and breathing are both absent start CPR (Cardio Pulmonary Resuscitation).
CLICK HERE FOR 👉 SAFETY INDUCTION, EDUCATION, AND TRAINING
Head Foot Exam= If both neck pulse and breathing are present and the patient is responding, continue with head to foot examination. Look for injuries bleeding and fractures systematically. Especially look for injuries on the head, chest, and abdomen. They may not look important in beginning but may prove to be fatal in the long term.
Use the First Aid equipment, if available. All passenger trains, some Railway Stations, lorries, and buses keep them. Make use of the material so obtained. On most occasions, the standard First’ Aid equipment will not be available. You will have to depend on the material at hand and improvise them for your requirements.- In a factory, use the prescribed first aid box.
Inspect the area. Take the casualty away from live wires, fallen walls, beams, fire, broken gas chambers, moving machinery, etc. to a safer place.
Clear the crowd with nice words. Do not allow people to crowd around the casualty. The casualty needs fresh air. If a doctor is present, he will guide you. Any other First Aider must be asked to help. Otherwise, take the assistance of bystanders giving them correct instructions.
CLICK HERE FOR 👉 How to Make Emergency Response Plan for Construction Site.
Note the weather. If it is fine, i.e. without rain or heat or a cold breeze, treat in the open. Otherwise, move the casualty into an airy room. If no suitable house or a doctor’s clinic is not nearby, it is best to protect the casualty with an umbrella or a sheet of cloth or even a newspaper.
Reassure, the casualty. Soft words and encouraging talk will make the casualty take things easy and lie quietly. These will help recovery.
Arrange for dispatch to the care of a doctor or to the Hospital. At the same time intimate the relatives where the casualty is being taken to.
Do not attempt too much. You are only a First Aider. Give minimum assistance so that the condition does not become worse and life can be saved.
The first aider should know the proper use of antiseptic, aseptic, and sterilized dressing material, surgical instruments and syringes. Some commonly used chemical antisepsis (to kill microorganisms in the wound) are: Hydrogen peroxide solution. Potassium permanganate. Boric acid. Tincture of Iodine, lodinate, lodoform, Chloramine B, Mercuric chloride. Dioxide, CoUargol, Silver nitrate. Spirit (ethanol). The brilliant green solution, Methylene blue solution, Degmin, Ethacrdidme lactate, Furacilin, Ammonium hydroxide solution, pure- phenol (carbolic acid). Formaldehyde solution and Sulphonamides.
CLICK HERE FOR 👉 How to Make Safety Plan for Construction Site.
Ten commandments of First Aid:
Dr. Subhash Mhaskar of Thane has highlighted in his small pocket-book, the ten commandments of First Aid as under:
- You shall always try to help the casualty to the best of your knowledge and with sympathy.
- Never give anything by mouth to an unconscious patient.
- Always keep the unconscious patient in the recovery position.
- Always look for breathing and pulse. If it stops, start CPR (Cardio Pulmonary Resuscitation) without any loss of time.
- In an unconscious patient with poisoning, never induce vomiting.
- Do not add Haldi, chuna or any other thing in a wound.
- In a poisonous snake bite, tie a tight bandage before everything and do not release it till the patient is taken to a doctor. The bandage should not block arterial circulation.
- When neck spine fracture is suspected, absolutely do not allow to move the neck. It can cause instant death.
- Do not give CPR to a conscious patient.
- Always take the patient to a doctor. Do not try to take place of a doctor.
Semi or fully automatic external defibrillator should be provided at all prime places, factories, OHC, medical centers, etc. It is most useful in cases of cardiac toxicity and sudden heart arrest.
CLICK HERE FOR 👉 Safe Handling and Storage of Ammonia
INJURIES AND FIRST AID AT A GLANCE
Injuries may be as follows:
The victim may be pinned down under the machinery. There may be lacerations; a part of a limb may be avulsed, there may be multiple fractures of severe traumatic shock. In some cases, it is not possible to extricate or release the victim.
In such cases, the machinery should be stopped immediately, power cut off and services of senior forman or the person who is familiar with the machine, requisitioned. Modern machines have automatic releasing devices or you may have to dismantle the parts.
The first aider is to attend the victim, control the bleeding, treat shock, reassure and cover any burnt or injured part. If the victim is unconscious ensure that the airway is clear. Arrange for immediate medical aid at the spot and remove it to the hospital.
Burns due to chemicals or hot substances, cuts, wounds, shocks, bleeding, unconsciousness, poisoning, and casualty may also happen which should be properly approached.
Some typical injuries and first aid for them are briefly described below to study them at a glance.
First Aid for Shock:
- Lay the patient on his back. The lower head end.
- Stop bleeding if any. Stop pain in burns by pouring cold water.
- Relieve pain by supporting the injured part.
- Keep the patient comfortable, but not hot. Do not cause sweating.
- Make the air passage clear and clean.
- Fluids may be given in small amounts unless the patient, is nauseated, unconscious, likely to be operated on, or has an abdominal wound.
- Reassure and cheer up the patient.
CLICK HERE FOR 👉 Handling of Corrosive Chemicals
First Aid for Electric Shock:
- Separate the patient from the electric current by proper technique. Stop the switch or use a wooden stick for separation.
- Make a rapid examination to ensure that the air passages are free. Clean them if necessary.
- Restore natural breathing by artificial respiration, if breathing has ceased.
First Aid for Wounds:
- Stop the bleeding by any one of the following methods:
- Direct pressure.
- Direct finger pressure into the wound in case of the larger bleeding wounds.
- Tourniquet (seldom needed) use only as a last resort.
- Avoid touching the wound with hands or unsterile material.
- Clear the wound with running water and surrounding area with soap or spirit with clear gauze washing away from the wound. Apply ready-made adhesive gauze bandage or sterile gauze and roller bandage as needed.
- Keep the patient quiet; raising the extremity if it is the bleeding part. Give no stimulants.
- Never apply antiseptic ointment, lotion or iodine or germicide to the wound.
- Elevate the injured part above the patient’s heart level.
- Try and use rubber gloves.
CLICK HERE FOR 👉 Heatstroke treatment
First Aid for Abdominal wounds:
- No time must be lost in sending the patient, to the hospital.
- Keep the patient flat.
- Give nothing by mouth.
- Maintain warmth.
- If. intestines protrude from the wound do not attempt to touch or replace them.
- Apply sterile dressing and binder as for wounds.
- Provide careful and immediate transportation to the hospital.
First Aid for Eye-Wounds:
- Removal may be attempted if the foreign body is not embedded.
- Do not apply- oil or ointment.
- If there is a foreign body embedded in the eyeball, send the patient immediately to the doctor after applying pad and loose bandage.
First Aid for Chemical Burns of the Eyes:
- Immediate washing of the eye at least for fifteen minutes is of great importance.
- Apply a sterile bandage and send the patient immediately to the doctor.
- Neutralizing agents or ointment should not be used.
First Aid for Suffocation:
- Remove the patient from the source of danger.
- Make a rapid examination to ensure that the air passages are free and to clean them if necessary.
- Restore natural breathing by artificial respiration, if breathing has ceased.
First Aid for Infection:
- Wash hands with soap and water.
- Use diluted antiseptic like diluted Dettol/savlon.
- Cover the wound with a sterilized bandage or clean cloth.
- Do not tighten the bandage excessively.
- Do not apply haldi, lime, etc. on the wound.
CLICK HERE FOR 👉 Artificial respiration
First Aid for Heatstroke:
- Make the patient lie down.
- Remove all clothing except underwear.
- Pour cold water on the head and body.
- Keep the patient under the fan.
- Record the temperature every 10 minutes and when it falls up to 30 °C, stop pouring water and clean the head and body with a towel.
- Give plenty of cold water with a spoonful of common salt in a glass of water to drink.
First Aid for Bleeding Nose:
- Make the patient sit with the head downward.
- Pinch the nose with fingers and thumb.
- Apply ice or cold compressing or pour cold water on the head.
- Do not plug the nostrils.
- Do not put water or any medicine through the nostrils.
- Send for medical attention.
First Aid for Bleeding Ear:
- Lay the patient with the head slightly raised.
- Incline the head to the affected side and apply a dry dressing over the ear with a loose bandage.
- Do not plug the ear.
- Apply pressure in front of the ear.
- Seek medical attention.
First Aid for Insensibility:
- Send it to a doctor. Meanwhile, do the following:
- Where the patient’s face is pale, lay him flat and face downwards with his head turned to one side. If his face is flushed or blue, raise and support the head and shoulders.
- Control any serious bleeding.
- Loosen any tight clothing and let him have plenty of air.
- Do not give anything by mouth.
- If the doctor is not available to send the casualty to the hospital.
CLICK HERE FOR 👉 OIL AND GAS SAFETY OFFICER INTERVIEW
First Aid for Heart Attack:
It is very important that the heart attack patient reaches the hospital in the first 2 hours.
The important symptoms of Heart Attack are:
- Symptoms (3Ps):
- Pain in chest: In the center of the chest radiating to left arm, jaw or left shoulder. The pain is consisting, severe and lasts for more than 5 minutes.
- Perspiration: Sudden, severe perspiration without cause.
- Palpitation: Without exertion.
- Sudden vomiting with gases like symptoms but with restlessness and perspiration.
- Sudden breathlessness.
In case of mild heart attack:
- Stop all activities of the patient.
- If available keep Sorbitrate tablet under the tongue of the patient.
- Give half an Aspirin tablet.
- Watch for pulse and breath.
- Contact the doctor immediately.
In case the patient becomes unconscious and breathing and neck pulse stop, immediately call for help and start C.P.R. as per instructions.
CLICK HERE FOR 👉 SAFETY AT CONSTRUCTION SITE
Epilepsy:
- Open the airway.
- Prevent tongue biting.
- Keep the patient in recovery position till consciousness
Bruises
- Cold applications in the first 24 – 48 hours.
- Later heat after 24 – 48 hours.
Burns :
- Act quickly.
- Put the affected part in cold water.
- Pour water on burns that cannot be immersed (Coldwater relieves pain, reduces fluid loss).
- Cover with a sterilized dressing.
First Aid for Dog Bite:
- Wash the wound immediately with water or Dettol.
- Do not try to stop bleeding.
- Cover the wound with a sterile dressing.
- Send the patient to the hospital.
- Watch the dog for 10 days.
First Aid for Snake Bite:
- Advise the patient not to panic and run.
- Without delay tie a band or handkerchief tightly 2-4 inches above the bitten part. However, you should feel a pulse below the bitten part.
- Lower the bitten part below the heart.
- Wash the bitten part with clean water.
- Examine the pulse and respiration.
- Carry the patient to the hospital for antisnake venom injection.
- If possible cut at the wound with a snake bite insect, knife or a sharp instrument to allow free bleeding.
- Never suck the blood from the wound.
First Aid for Unconsciousness or Coma:
Main cause – Head injury, brain diseases, poisoning, asphyxia, heart attack.
Treatment:
C: Call for help. Lie down the patient in a prone position.
O: Observe the patient’s breathing, heartbeat, and pulse.
M: Maintain a recovery position. Loosen tight clothing. Clean the airway. Give artificial respiration or external cardiac massage.
A: Absolutely nothing by mouth. Arrange for transport to the hospital immediately.
FIRST AID IN MINOR AND CLOSED INJURIES
Minor Injuries:
Minor injuries (cuts, punctures, abrasions, scratches, splinters) are frequent in everyday life. In themselves, they are not dangerous and do not cause loss of working, ability but when first aid is not properly rendered they can be complicated by purulent inflammation.
Any break in the skin, even in minor injury, should be painted immediately with a 5 percent iodine tincture and covered with an aseptic bandage.
If the skin and wound are contaminated, the skin around the wound should be wiped with 0.5 percent ammonium hydroxide and the wound with 3 percent hydrogen peroxide. When the edges of the wound are smooth and even but the wound is wider than 0.5 cm its edges should be brought together.
For that purpose, a piece of adhesive plaster shorter than the wound is cut from a strip and one end .is stuck across one edge of the wound to the skin, the opposite edge of the wound is brought close and fixed by the other end of the plaster.
The plaster should not wholly cover the wound, and its ends should be left uncovered. An aseptic bandage is then applied to the wound over the plaster. Minor wounds and abrasions are covered by colloid or special glue.
CLICK HERE FOR 👉 PREVENT ROAD ACCIDENTS
It is desirable to cover punctured wounds with a spirit bandage.
With contusion of the fingers or toes, there is often bleeding beneath the nails that later can suppurate and cause acute inflammation. To prevent this complication it is necessary for a doctor to release the blood accumulated under the nail and apply a spirit bandage.
The procedure is simple and does not require anesthesia. When foreign bodies (clearly visible metallic needles, filings or chips, splinters of wood, etc.) penetrate the skin they should be removed by tweezers, the wound painted with iodine tincture and a spirit bandage applied.
Closed Injuries:
Closed traumas are mechanical injuries in which the skin and mucous membranes are not broken. They include contusions of various parts of the body (and the skull and brain), strained ligaments, dislocations, subcutaneous rupture of the muscles, internal organs of the chest and abdomen and bone fractures. Bruises and contusions may be caused by a blow from a blunt object or by falling.
The signs include pain at the site of the injury and the development of a bruise which becomes bluish in a few days.
First Aid: In order to lessen the pain and to prevent bleeding the contused area should be immobilized, raised and cooled by applying an ice bag or acold compress. The cold contracts the blood vessels and reduces bleeding.
Two or three days after the bruise warmth should be applied to accelerate the resolution of the effused blood (hot compresses, local warm baths).
CLICK HERE FOR 👉 Near-miss related to falling of objects
A hot compress (fomentation) is made as follows: A folded pad of cloth is soaked in water, an 8 percent solution of surgical spirit or camphor oil, wrung out and applied to the skin.
An oilskin or waxed paper of a larger size (two or three centimeters larger than the compress) is laid over it and the whole is covered by a thick layer of cotton wool and secured with a roller bandage. The compress is left for six to eight hours, during which the moist layer dries. After the compress is removed the skin is wiped with alcohol.
Sprains of ligaments are frequent. An awkward movement wrenches joint or a slip overextends a joint which causes some degree of tearing of the joint capsule or ligaments.
Pain and swelling develop around the joint but its outlines are generally not noticeably altered. The victim can use his limb, but with difficulty. Put weight on the foot or move the painful arm. After a few days, the skin becomes black and blue.
First Aid: The affected limb should be immobilized (an arm put in a sling made from a triangular bandage and affected ankle tightly bandaged),. After two or three days, treatment is begun (hot compresses, local warm baths and massage).
CLICK HERE FOR 👉 RADIATION SAFETY
A dislocation is a more serious injury attended with rupture of the joint capsule and displacement of the joint surfaces of the articulated bones.
First Aid: A fixing bandage or a splint is applied and the patient sent to the hospital for the dislocation to be reset.
Fractures:
It may be open or closed. Open fractures in which not only the bone but also the skin is damaged are most dangerous. Germs can get into die wound formed by the break in the skin and cause suppuration gas gangrene or tetanus. In closed fractures, the outer coverings (skin and mucous membranes) are intact and prevent the entry of germs.
The signs of fractures of the long tubular bones include pain, hemorrhage, distortion of the injured part of the arm or leg, abnormal mobility in a place where there should be none, crackling, swelling, deformity, and inability to make any movement.
The fragments of the bone may be displaced to a varying degree in length, width, or at an angle to each other causing some deformation of the limb.
First Aid: The limb affected must be immobilized. This is especially important during the transportation of the patient. The bone fragments should be tied so that they cannot move. The rules for immobilizing fractures should be observed. If they are not observed, grave complications can develop menacing the patient’s life.
Treatment:
- Immobilize the fractured limb with splints like a wooden stick, hardboard or umbrella.
- Make padding of cotton or hanky on the splints.
- Do not tighten the splint too tight or loose.
- Elevate the injured limb.
- Use natural splints, like if a leg is fractured the other leg can be used as a natural splint.
CLICK HERE FOR 👉 Workmen’s Compensation Act and Rules 1923 1924
Spine Fracture:
Falling from height can cause spine fracture
Treatment:
Move the patient on a hard surface like table or bench etc.
- Do not allow to sit, stand or walk.
- Tarn the patient by log rolling.
- Shift the patient to the hospital.
Backbone (Spinal) Fracture:
- Transport on a rigid frame. This frame may be improvised by using available boards or a door.
- The rigid frame may be placed on a stretcher for transportation.
- If a firm frame cannot be improvised, transport the patient on the abdomen on a stretcher made of canvas or blanket.
- In neck fracture cases it is much better to get a doctor to the scene because the danger to life is great.
- Immediate hospitalization is necessary.
Foreign Body in the Body Part:
Foreign Body under the Skin:
Thorns, glass, iron, pieces, needles, etc., get under the skin.
First Aid:
- Unless very easy to deal with, don’t interfere.
- Dress the wound.
- Immobilize the part with splints and get medical aid.
Foreign Body in the Eye:
Wings of insects, dust, coal (from boilers -etc.), metal particles from lathes and loose eye-lashes are common objects which get lodged under the eyelids. They cause pain and later redness if they are not removed at once. Sometimes iron particles and wood splinters get lodged in the corner causing serious trouble. Penetrating foreign bodies, however, are a danger to the eye itself.
CLICK HERE FOR 👉 EMPLOYEE PARTICIPATION IN SAFETY
First Aid:
- Avoid rubbing the eyes. In case of a child, tie his hands at the back.
- Seat the casualty so that light falls on the eye. Pull the lower lid down. If the foreign body is floating and not embedded, remove it with a narrow, moist swab. The corner of a handkerchief twisted to a fine point will also do.
- If the foreign body is not visible it may be under the -upper eye-lid. Ask the casualty to keep clean water in the hand and blink briskly in the water. If unsuccessful, pull the upper lid forward, push the lower lid upwards and let go of both the lids. The lashes of the lower lid usually dislodge the foreign body. Try this two or three times.
- If the foreign body is embedded in the eye, particularly the cornea (the black of the eye) do not touch it—apply a soft pad, bandage the eye, ask the casualty not to rub the eye and take him immediately to a hospital.
- Penetrating foreign bodies are easily made out of bleeding, pain, etc. It is for the doctor to handle. You just put a pad bandage.
- When corrosive acid, alkali or juices from plants are suspected, blinking eyelids under water a number of times or flushing with a large quantity of water is the best thing to do. Then apply a soft pad, tie a bandage (not tightly) and take the casualty to the hospital at once.
Foreign body in the Ear:
- If it is an insect, fill the ear with glycerine or coconut/mustard oil or warm saltwater. The insect will float up and can be removed easily.
- If there is nothing floating up, leave it alone, don’t meddle at all but take him to a doctor.
- If it is solid, do not try to remove, scratch or probe it. Take him to a doctor.
Foreign Body in the Nose:
- Do not interfere with the foreign body.
- Make casualty breathe through the mouth.
- Take him to the hospital. If a child, tie the hands behind so that he does not interfere with the foreign body.
Foreign Body in the Throat:
- Some small objects like a safety pin sometimes get stuck in the throat. A draught of water is all that is needed to pass it further down.
- Some irregular objects, fairly large, get stuck. If visible they can be taken out with the fingers. If a child, holds it up, head downwards and tap on the back of the neck, the foreign body will fall out.
- Fish-bone or thorn get lodged by piercing some part of the throat. Keep the relatives and the casualty quiet and remove the casualty to the hospital at once.
CLICK HERE FOR 👉 Heinrich’s Theory of Accident
Foreign Body in the Stomach:
Smooth objects like coins, buttons, nuts, safety pins are swallowed.
- The stomach and intestines will adjust themselves in such a way as to throw them out.
- Do not panic.
- Show the case to a doctor.
- There is no need to give laxatives (or bananas as is usually done).
Dressing & Bandaging:
A dressing is a protective covering applied to a wound to
- Prevent infection.
- Absorb discharge.
- Control bleeding and
- Avoid further injury.
An effective dressing should be sterile (germ-free) and porous to allow for oozing and sweating.
The dressing should be applied gently after washing hands thoroughly. No part of the wound or dressing to be contacted should be touched by fingers. Dressing must be covered with adequate pads of cotton wool, extending well beyond them and retained in position by a bandage or strapping.

Bandages are made from cotton cloth, elastic net or special paper and are used to (1) retain dressings and slings in position (2) maintain direct pressure over a dressing to control bleeding (3) prevent or reduce swelling (4) provide support for a limb or joint (5) restrict movement and (6) assist in lifting and carrying casualties.
CLICK HERE FOR 👉 Directing For Safety
Bandages should not be too loose or too tight. A bluish body part or loss of sensation indicates too much tightening.
Bandages are of two types – Triangular and Roller bandages.
A triangular bandage is made by cutting a square piece of cloth 100 cm~ from corner to corner so as to give two bandages. A triangular bandage can be used (1) as a whole cloth spread out fully and (2) as a narrow bandage by folding to the required size. For tying the bandage a ‘reef knot’ should be used and not a ‘granny knot’ which is likely to become loose.
There are systematic methods of bandaging with the triangular or roller bandages.
Triangular bandages can be used for scalp, forehead, eye, cheek, front or back of the chest, shoulder, elbow, hand, hip or groin, knee, foot, and stump.
Roller bandages are made of cotton with loose mesh, are of various lengths and widths and are used in hospitals and first-aid posts. Roller bandages should be applied firmly and evenly. There are 4 methods to apply roller bandages (1) Simple spiral (2) The reverse spiral (3) Figure of Eight and (4) The Spica.
ELECTRICAL INJURIES
Causes of Electrical Injuries: If any part of the body comes in contact with a “live” wire which is exposed and not covered by an insulator, or with a cable or rail in which current is leaking, a person gets an electric shock.
In houses, the blowing out of switches or fuses or faulty electrical connections can cause such injury. The injury may be quite mild or so severe as to cause immediate death. Electrical shock is produced only when an electric current passes through the human body which is in contact with the earth. It passes even more quickly if the part is wet.
In wet conditions, the even lower voltage may be dangerous. A very strong current passing to earth through lower limbs may be less dangerous than a weaker current passing through the chest, especially so when it enters through the hands and arms.
CLICK HERE FOR 👉 Planning for Safety
The Effect of Electric Shock.
- There may be fatal paralysis of the heart.
- There may be a sudden stoppage of breathing due to paralysis of muscles used in breathing.
- The heart may continue to beat, while breathing has stopped. In this condition, the face appears blue.
- There may be burns, either superficial or deep. They depend on the strength of the electric current causing the injuries.
First Aid: Intelligent and prompt action is required. If the first aider is not cautious, he may also receive a severe electric shock or even die along with the casualty.
- If the casualty is still in contact with the conductor, switch off the current. If the switch is not found, remove the plug or cut off the current by breaking the wire, ensure that you stand on a dry piece of wooden board. Do not use scissors or a knife. The wooden handle is unsafe above 380 V. When the current is of low voltage the first aider should stand on an insulating material that is dry. (Insulating materials are rubber-soled shoes, wooden plank or piles of newspaper). High voltage rubber gloves should be worn. If not, a dry coat, cap or other clothing may be used. When the current is of a very high voltage, as in the case of overhead (high tension) lines, there is a greater danger. The casualty may not be in actual contact with the wire as the current can pass through the gap (causing an arc). The first aider in such circumstances should keep as far away as possible from the electric wires. The casualty is to be dragged out by means of a non-conducting material. A walking stick, dry bamboo pole, wooden plank or a dry rope is to be used.
- If the casualty is not breathing normally, or heart has stopped beating, open his clothes, unbutton the collar, loosen the belt, give artificial respiration and external cardiac massage for a long time.
- Treat for shock.
- Treat for burns if any.
- Transfer to a hospital or seek the help of a medical practitioner who is nearest.
- Even when the casualty has recovered fairly well after first aid is given, he must be examined by a medical specialist because electric injuries are liable to relapse.
CLICK HERE FOR 👉 Chemistry and Pyramid of Fire
ARTIFICIAL RESPIRATION
Treatment when not breathing:
- Loosen all clothing at waist, chest, and neck.
- Tilt the head backward, while supporting the back of the neck with your palm. This will lift the tongue to its normal position. Thus the air passage will be cleared and the casualty may begin to breathe after a gasp.
- If breathing does not begin after the above treatment, help movements of chest and lungs four or five times. This will be usually enough to start breathing. If breathing does not start even now, mouth to mouth (-to-nose) breathing should be begun.
Mouth-to-Mouth breathing:
- Place the casualty on his back. Hold his head tilted back.
- Take a deep breath with mouth open wide.
- Keep nostrils of casually pinched.
- Cover the mouth of the casualty with your mouth smugly.
- Watching the chest, blow into his lungs until the chest bellows up. Withdraw your mouth. Note the chest falls back (It is hygienic to cover the mouth of the casualty with your handkerchief or some clean cloth).
- Repeat the above 15 to 20 times a minute.
- If the casualty is young (baby or child) the operations areas above, but your open mouth should cover both the mouth and nose of the casualty and blow gently.
- If the chest does not rise (as in 5 above) look for an obstruction.
- Turn the casualty to a side and thump his back. This will make the obstructing material come to the front of the throat. Open the mouth and remove it with your finger covered with a piece of the cloth.
- If a child, hold it up by the feet and thump the back.
- Use mouth-to-nose respiration if mouth-to-mouth is not possible, but now the casualty’s mouth should be closed by the First Aider’s thumb.
- If the heart is working, continue artificial respiration until normal breathing occurs. Send for Ambulance.
- If the heart is not working, you will notice:
- The face is blue or pale.
- Pupils are dilated.
- Heartbeats and pulse at the root of the neck (carotid) are not felt.
- Then treat as follows: (a) Place the casualty flat on his back on a hard surface (bench, table, etc.) (b) Give a smart hit with the edge of your hand on the lower and left angle of the sternum. This usually stimulates the heart to work. (c) In case the heart does not work, persist the striking for 10-15 seconds at the rate of one stroke a second. Feel for the pulse at the root of the neck all the time. If the pulse becomes regular and continuous, stop beating, all the while artificial respiration has to go on.
Even if the casualty is breathing, but breathing is not normal, it is wise to start artificial respiration. Do not begin thumping the heart or compression until you are sure that the heart has stopped beating.
External Heart Compression:
(If there are two trained persons):
- This should go on along with artificial respiration. Therefore ask the First Aider giving mouth-to-mouth breathing to sit to the right of the casualty and place yourself on the left side.
- Feel and mark the lower part of the sternum.
- Place the heel of your hand on the marked part (make sure that the palm and fingers are not in contact with the chest).
- Place the heel of the other hand over it.
- With your right arm, press the sternum backward, towards the spine. (It can be pressed back 1 to 1.5 inches in adults).
- Adults should be given about 60 pressures a minute. For children from two to ten years, 3 pressures with one hand (heel) will be enough, but pressure should be 80 to 90 times a minute. For babies up to two years, 2 pressures with two fingers are good enough if applied 100 times per ” minute.
- Press firmly but carefully. Carelessness (overpressure) may cause injury to ribs and deeper tissues.
- If the treatment is effective (a) Colour will become normal (b) Pupil will contract as improvement beings: and (c) Carotid pulse begins with each pressure.
- When the pulse is not restored, continue compression until the patient reaches the hospital.
- The inflation of lungs to heart pressure should be as 2.15. If there is only one First Aider, he has to be very smart and active. Finish 15 heart compression, rush to head-side, give two inflation to the lungs, and get back to the heart and give 15 compressions. Repeat these. If there are two First Aiders, No. 1 makes 5 heart compression and then No. 2 gives two lungs inflation. These are repeated. At the same time, No. 1 can watch the pupils and No. 2 can feel the carotid pulse.
CLICK HERE FOR 👉 Work Permit System
BURNS AND SCALDS
Causes of Burns and Scalds:
- Burns are injuries that result from dry heat like fire, flame, a piece of hot metal, the sun, contact with a wire carrying high tension electric current or by lightning or friction. Scalds are caused by moist heat due to boiling water, steam, oil, hot tar, etc.
- Chemical burns are caused by strong acids (Sulphuric acid. Nitric acid etc.) or by strong Alkalis (Caustic Soda, Caustic Potash, quick lime or strong Ammonia).
- A nuclear burn is caused by the instantaneous flash of intense heat given off by a nuclear explosion. It is capable of causing superficial burns on the exposed skin of persons several miles away.
Degrees or Depth of Burns:
The degrees of burns indicate the degree of damage to the tissues. There are five degrees of burns:
First Degree: When the skin is reddened
Second Degree: When there are blisters on the skin, and
Third Degree: When there is the destruction of deeper tissues and of charring.
Fourth Degree: Steam blebs
Fifth Degree: Carbonisation
Percentage of Burn:
The danger from burns depends on the area i.e. the percentage of the body part of the burns rather than the degree. Superficial burns over a large area of the body are more dangerous than the complete carrying of a part of the limb. It must be noted that in the same person, different parts of the body may show different degrees of burns. Any burn of over 30% irrespective of deep degree – should be hospitalized as a priority. More than 50% of burns are more serious.
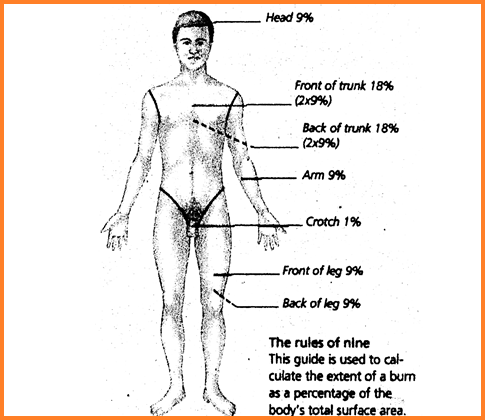
The above figure shows the percentage (extent) of burns. It follows the rule of 9. For more area, add the percentage appropriately. For example, burns of both hands and both legs indicate 9+18 = 27% burns.
CLICK HERE FOR 👉 HISTORY OF THE SAFETY MOVEMENT AND THE FACTORIES ACT
Helping a person whose clothes have caught fire:
The First Aider should know how to deal with a person whose clothes have caught fire.
- Put out the flames by whatever means available. Most of the causes of burns occur in homes and drinking water is readily available to quench the flames, water also cools the burnt area causing less damage to occur.
- Do not allow the person to run about. This only fans the fire and makes the flames spread.
- Hold a rug, blanket, coat or table cover in front of you, while approaching a man whose clothing has caught fire.
- Lay him down quickly on the ground and wrap tightly with any thick piece of cloth, rug or coat. Smother the flame by gently rolling the causality or by gentle pats over the covering.
- If the clothes in front of the body have caught fire, lay him on his back and vice versa, till suitable material is brought to smother the flame.
Rescuing Persons from Fire:
- In rescuing persons from a room that has caught fire, quick and clear thinking is required.
- Remember clean air is at ground level. So crawl along the floor to pull out a person who is lying unconscious or is disabled.
- Have a wet kerchief around your face when you go for the rescue.
- If there is carbon monoxide in the room, these precautions do not protect the rescuer from carbon monoxide poisoning. When there is a fire in a closed room, there is always some amount of carbon monoxide, therefore quick action is all-important.
- When there is the fire in a room in which the doors and windows are closed, do not open the windows and door to let in air. The rush of air will increase the fire and it will burn more intensely.
First Aid of minor Burns and Scalds:
In the case of minor burns:
- Clean the area gently with clean water.
- Submerge the burned area in cold water.
- Apply a solution of salt and water (one teaspoonful to a pint of water) is out of the way places.
- Cover with a dry dressing.
- Do not apply cotton wool direct to the burnt.
- Do not apply any greasy substance.
- Give warm drinks for example sweetened tea or coffee.
First Aid of Serious Burns and Scalds:
Immediate attention that required in serious burns are:
- Keep the casualty quiet and reassure him.
- Wrap him up in clean cloth.
- Do not remove adhering particles of charred clothing.
- The cover burnt area with a sterile or clean dressing and bandage. In case of burns covering a large part of the body, it is sufficient to cover the area with a clean sheet or towel.
- Keep him warm but do not overheat him.
- If the hands are involved, keep them above the level of the victim’s heart.
- Keep burned feet or legs elevated.
- If the victim’s face is burnt, sit up or prop him up and keep him under continuous observation for breathing difficulty. If respiratory problems develop, an open airway must be maintained.
- Do not immerse the extensive burned area or apply ice-water over it because cold may intensify the shock reaction. However, a cold pack may be applied to the face or to the hands or feet.
- Shift the casualty to the nearest hospital if he is fit to be moved.
- If you cannot take him to a hospital, wait for the doctor to arrive.
- Do not open blisters.
- Keep him wrapped up in clean cloth.
- Treat for shock.
- Remove quickly from the body anything of a constricting nature like rings, bangles, belt, and boots. If this is not done early, it would be difficult to remove them later as the limb begins to swell.
- If medical help or trained ambulance personnel cannot reach the scene for an hour or more and the victim is conscious and not vomiting give him a weak solution of salt and soda at home and en route :- One level teaspoonful of salt and half level teaspoonful of baking soda to each quart of water, neither hot nor cold. Allow the casualty to sip slowly. Give above four ounces to an adult over a period of 15 minutes: two ounces to a child between 1 and 12 years of age and about one. ounce to an infant under one year of age. Discontinue fluid if vomiting occurs. Do not apply ointment or any form of grease or another home remedy.
First Aid of Chemical Burns:
- Wash off the chemical with a large quantity of water for 15 minutes by using a shower or hose if available as quickly as possible. This flooding with water will wash away most of the irritants.
- Cut out contaminated clothing.
- Do not touch.
- Treat as for burns.
Burns of the Eye:
Acid Burns:
- First aid for acid burns of the eye should be given as quickly as possible by thoroughly washing the face, eyelids and the eye for at least fifteen minutes by water.
- If the casualty is lying down, turn his head to the side, hold the eyelids open and pour water from the inner corner of the eye outward. Make sure that the chemical does not enter into the other eye. Cover the eye with a dry, clean protective dressing (do not use cotton) and bandage.
- Neutralizing agents or ointments should not be used.
- Caution the victim against rubbing his eye.
- Get medical help immediately (preferably an eye specialist).
Alkali Burns:
Alkali burns of the eye can be caused by drain cleaner or other cleaning solutions. An eye that first appears to have only a slight surface injury may develop deep inflammation and tissue destruction and the sight may be lost.
CLICK HERE FOR 👉 ACCIDENT CAUSATIVE FACTORS
- Flood the eye thoroughly with water for 15 minutes.
- If the casualty is lying down, turn his head to the side. Hold the lids open and pour water from the inner corner outward. Remove any loose particles of dry chemicals floating on the eye by lifting them off gently with a sterile gauze or a clean handkerchief.
- Do not irritate with soda solution.
- Mobilize the eye by covering with a dry pad or protective clothing. Seek immediate medical aid.
POISONING, FIRST AID AND ANTIDOTES
Some substances when taken into the body in fairly large quantities or lethal doses can be dangerous to health or can cause death. Such substances are called poisons.
Poisons get into the body by swallowing or by breathing poisonous gases, or by injection through the skin.
Poisoning by Swallowing (Mouth route):
Sometimes acids, alkalis, disinfectants, etc., are swallowed by mistake. They burn the lips, tongue, throat, food passage and stomach and cause great pain.
Other swallowed poisons cause vomiting, pain and later on diarrhea. Poisonous fungi, berries,’ metallic poisons and stale food belong to the latter group. Some swallowed poisons affect the nervous system.
To this group belong (a) alcoholic drink (methylated spirit, wine, whiskey, etc.) when taken in large quantities, and (b) tablets for sleeping, tranquilizers, and pain-killing drugs (Aspirin or Largectil). All these victims must be considered seriously ill.
The symptoms are either delirium or fits or coma (unconsciousness). Some poisons act on the nervous system (belladonna, strychnine).
Poisoning by Gases (Nose route):
Fumes or gases from charcoal, stoves, household gas, motor exhausts, chemicals and smoke from explosions, etc.; cause choking (asphyxia) which may result in unconsciousness in addition to difficulty in breathing.
Poisoning by Injection (Skin route):
Poisons get into the body through injection, bites of poisonous snakes and rabid dogs or stings by scorpions and insects. Danger to life is again by choking and coma.
CLICK HERE FOR 👉 HIRA
General First Aid in Poisoning:
- Poisoning is a serious matter. The patient must be removed to a hospital/or a doctor be sent for, at once with a note of the findings and, if possible, the name of the poison.
- Preserve packets or bottles which you suspect contained the poison and also any vomits, sputum, etc.. for the doctor to deal with.
- If poison is’ not known: Make a quick assessment of the likely route of exposure by examining the eyes, mouth, nose, and skin of the victim for signs of the chemical itself or damage it has caused such as swelling, redness, bleeding, burns, discharge of fluid or mucous or pallor. Drooling, difficulty in swallowing, a distended, painful, hard, or rigid abdomen all indicates possible ingestion of a corrosive or caustic substance. If respiration is rapid, shallow, noisy or labored, suspect inhalation. If the face has been splashed with chemicals, eye contact is likely.
- Poisoning by inhalation: Remove victim from exposure while protecting yourself from exposure. If breathing has stopped, administer artificial respiration using a bag-valve-mask. Do not use mouth to mouth resuscitation. Instead, use the chest pressure-arm lift technique. Maintain an open airway. Arrange for transport of the victim to a medical facility.
- Poisoning by Ingestion: Do not induce vomiting if he has abdominal pain or burns in the mouth. If no such problem, then induce vomiting by syrup of ipecac. Lastly, give 1 or 2 cups of water to drink.
- Poisoning by skin contact: Remove the victim from the contaminated area: Be careful to protect your lungs, skin, and eyes while doing so. Remove the victim’s clothing, shoes, and jewelry from the affected areas, cutting them off if necessary. Do this under a shower or while flushing with water. Continue to flush with water until all traces of the chemical are gone and any feeling of soapiness has disappeared also. Rinse for at least 15 minutes cover the victim with a blanket or dry clothing. Inform and refer the victim immediately to .a physician for his advice.
- In the case of inflammation, burns, blisters or pain– Loosely apply a dry sterile dressing if available or use a clean dry cloth for it. Inform and refer the victim immediately to a physician for his advice.
- If the victim is in a state of shock- Lay him down on his side and cover him with a blanket. Elevate his feet. Inform and refer the victim immediately to a physician for his advice. Do not break open blisters or remove the skin. If clothing is stuck to the skin after flushing with water, do not remove it.
- Do not rub or apply pressure to the affected skin.
- Do not apply any oily substance to the affected skin.
- Do not use hot water.
- Poisoning by eye contact: Remove the victim from the contaminated area. Be careful to protect your lungs, skin and eves while doing so. Act quickly. Flush the victim’s eyes with clean tepid water for at least 15 minutes. Has the victim lie or sit down and tilt his head back Hold his eyelids open and pour water slowly over the eyeballs starting at the inner corners by the nose and letting the water run out of the corners. The victim may be in great pain and want to keep his eyes closed or rub them but you must rinse the chemical out of the eyes in order to prevent possible damage. Ask the victim to look up, down and side to side as you rinse. Transport victim to the medical facility as soon as possible. Even if there is no pain and vision is good, a physician should examine the eyes since delayed damage may occur.
- If eyes are painful: a) Cover loosely with gauze or a clean, dry cloth. b) Maintain verbal and physical contact with the victim.
- If unconscious – (a) Do not induce vomiting (b) Make the casualty lie on his back on a hard, flatbed without any pillow and turn the head to one side. As there is no pressure on the stomach and the gullet is horizontal the vomited matter will not get into the voice box and the tongue will not close the air passage. This is also the best posture for giving artificial respiration, if needed (c) Sometimes when there is excess of vomiting the three-quarter-prone posture (i.e. the casualty is made to lie on his side with one leg stretched, the other bent at knee and thigh) will make things easier for the casualty (d) If breathing is very slow or stopped, start artificial respiration and keep it up till the doctor comes, (e) Maintain open airways (f) Do not use mouth to mouth re$uscitation (g) Do not give anything by mouth (h) In case of signs of shock, elevate-his feet, 20-30 cm and cover him with a blanket (i) Arrange for sending to medical facility.
- If conscious – (a) Aid vomiting by tickling the back of the throat or make him drink tepid water mixed with 2 tablespoons of common salt for a tumbler of water (b) Even if conscious when the poison is a corrosive do not induce vomiting. Signs of corrosives: Lips, mouth and skin show grey white or yellow, patches which are to be looked for: acids, alkalis, etc., cause such burns. First Aid: Factories that use certain poisons shall have the respective antidotes ready and displayed in an easily available place. The personnel should be taught about the use of antidotes – so that anyone can render assistance in case of emergency. The poison must be diluted by giving large quantities of cold water (chilled, if possible) This will dilute the irritant and delay absorption and will replace fluid lost by vomiting. Tender coconut water will be even better as this will be a portion of food and also a diuretic. Soothing drinks should be given. Milk, egg is beaten and mixed with water or sojee congee are good for the purpose.
CLICK HERE FOR 👉 PPE IS CODE
Alcohol Poisoning:
Alcohol taken in considerable (toxic) quantities may cause fatal poisoning, A fatal dose of ethyl alcohol is 8 g per I kg body weight. Alcohol affects the heart, blood vessels, gastrointestinal tract, liver, kidneys and mainly the brain.
In a case of severe intoxication, sleep is followed by an unconscious state. Vomiting and involuntary urination are frequent symptoms. The respiratory center is drastically inhibited, which is manifested by irregular breathing. Death ensues when the respiratory center becomes paralyzed.
First aid: Fresh air should be provided (a window open or the victim was taken outside) and vomiting induced by ‘minor lavage as’. If the patient is still conscious, he should be given hot strong coffee. A respiratory arrest is managed by artificial respiration.
Poisoning with Acids and Alkalis:
In poisoning with concentrated acids and alkalis, a grave condition rapidly develops, in the first place, to extensive burns in the mouth, throat, esophagus, stomach and often the larynx. Later, the absorbed toxins affect the vital organs (e.g. liver, kidneys, lungs, or heart).
Concentrated acids and alkalis are able to destroy tissues. The mucous membranes, being less resistant than the skin, are destroyed and necrosis occurs more rapidly involving deeper layers.
Burns and scabs form on the mucous membrane of the mouth and lips. In a bum due to sulphuric acid, the scabs are black, in a burn due to nitric acid they are greyish-yellow, in one due to hydrochloric acid they are yellowish-green and in one due to acetic acid greyish-white.
Alkalis more easily penetrate the skin and affect deeper layers. The burnt surface is loose, decomposed and whitish in color.
As soon as an acid or alkali is swallowed the patient feels a strong pain in the mouth, behind the breast bone and in the epigastrium.
When laid down he tosses in bed from unbearable pain. There is almost always tormenting vomiting often with admixtures of blood. Painful shock rapidly develops. The larynx may swell and asphyxia develops. When an acid or alkali is taken in great amounts, cardiac weakness and collapse rapidly develop.
Poisoning with ammonium hydroxide takes a grave course. The pain syndromes are attended by asphyxia because the airways are also affected.
The person -who is rendering first aid must find out at once which chemical caused the poisoning because the treatment varies according to the type of poison.
If the poisoning was caused by concentrated acids and the symptoms of oesophageal or gastric perforation are absent, the stomach should be leveraged through a thick stomach tube using for it 610 liters of warm water mixed with magnesium oxide (20 g per liter of liquid) or lime water.
Sodium carbonate is contraindicated for gastric lavage. “Minor lavage ” i.e. drinking 4-5 glasses of water and then inducing vomiting, will not alleviate the patient’s condition and sometimes may even promote absorption of the poison.
If a stomach tube is unavailable, the patient may be given milk, oil, egg, white, mucilaginous decoctions, or smoothing substances. In poisoning with carbolic acid (Phenol, Lysol) milk, oil or fat should not be taken.
Magnesium oxide mixed with water or lime water should be given in this case, as in poisoning by all other acids. Cold compresses or ice should be put on the epigastric region to lessen pain.
When the poisoning is due to concentrated alkalis, the stomach should be immediately lavaged with 6 10 liters of tepid water or a 1 percent citric or acetic acid solution within four hours of the poisoning.
When a stomach tube is unavailable and the patient’s grave condition (swelling of the larynx) prevents a stomach lavage, mucilaginous solutions are given, 23 percent citric or acetic acid solution (I tablespoonful every 5 minutes), or lemon juice. Rinsing of the mouth or administration of sodium hydrochloride solution is contraindicated.
The patient should be immediately admitted to a medical institution where he will be given the necessary urgent medical help.
It should be kept in mind that when a perforation of the esophagus or stomach is suspected, they were manifested by severe pain in the stomach and unbearable pain behind the breast bone, drinking and moreover, lavage of the stomach are not permitted.
CLICK HERE FOR 👉 SWL AND SAFETY FACTOR
Poisoning with Toxic Chemicals:
The latent course of the disease is 15-60 minutes, after which the symptoms of the affection of the nervous system appear (e.g. enhanced salivation, discharge of sputum and perspiration). Breathing accelerates and becomes noisy, as rail heard at a distance.
The patient becomes restless and excited. Cramp appears in the legs and the intestine undergoes increased peristalsis which is followed by muscular paralysis and paralysis of the respiratory muscles. The respiratory arrest that follows, causes asphyxia and death.
In accidents connected with the inhalation of the toxic chemicals, the victim must be immediately hospitalized. If possible, he should be given 6-8 drops of a 0.1 percent atropine solution or 1-2 tablets of belladonna.
When respiration is arrested, artificial respiration should be carried out. When the poisoning is caused by toxins getting into the gastrointestinal tract, the stomach should be washed with water mixed with a suspension of activated carbon Saline purgatives should also be prescribed. The toxic substances should be removed from the skin and mucous membranes with running water.
Carbon Monoxide Poisoning:
Carbon monoxide poisoning may occur in the chemical industry where it is used for synthesizing certain organic compounds (acetone, methyl alcohol, phenol etc.), in poorly ventilated garages, in furnaces or in stuffy, freshly painted premises. It may also happen in households when the stove shutters are closed too early in premises with stove heating.
The early symptoms are headache, heaviness in the head, nausea, dizziness, noise in the ears and palpitation. Later muscular weakness and vomiting occur.
If the victim remains in the poisonous atmosphere, the weakness intensifies, somnolence, clouding of consciousness and dyspnoea develop. The skin turns pale and sometimes bright red spots appear on the body. In further exposure to carbon monoxide the patient’s respiration becomes shallow, convulsions develop and paralysis of the respiratory center terminates in death.
First Aid: The victim must be immediately removed from the poisonous surrounding, better into the open air in warm weather. If his breathing is weak and shallow or arrested, artificial respiration should be continued until adequate natural breathing or the true signs of biological death appear.
Rubbing should be carried out and hot water bottles applied to the legs. A brief whiff of ammonium hydroxide is beneficial A patient with severe carbon monoxide poisoning must be immediately hospitalized in order to prevent possible grave complications in the lungs and nervous system which may develop later.
Antidotes for some common Chemicals:
Antidotes are therapeutic agents used to counteract the toxic effects of specific xenobiotics. These are heterogeneous groups of substances consisting of pharmaceuticals, biological agents and immunoglobulin fragments.
Different mechanisms of action are involved Some specifically act at the receptor sites while others exert their effect by changing the metabolism of the poison counteracting the toxic injury or just forming the inert complex with the poison.
Antidotes acting at receptor sites: Drug intoxications are mostly treated with these antidotes. However, Atropine is a specific antidote for organophosphate or carbamate pesticide poisoning. Similarly, physostigmine for Dhatura and neostigmine for Curare poisonings are useful. Others include naloxone for opioid, flumazenil for benzodiazepines and physostigmine for atropine poisoning.
CLICK HERE FOR 👉 SAFETY AUDIT
CLICK HERE FOR 👉 SAFETY COMMITTEE
Antidotes changing the metabolism of the poison: These antidotes either interfere with the metabolism of the toxic agent thereby reducing the toxicity or strengthen the detoxifying capacity of the body. Antidotes included in this group are ethanol, 4-methyl pyrazole, acetylcysteine, sodium thiosulphate, folinic acid, and pyridoxine.
Antidotes binding with the poison and forming less toxic complexes: In this category, poison may be adsorbed or chelated by the antidote. Activated charcoal effectively adsorbs a large variety of drugs and toxins, thereby decreasing their bioavailability and enhancing elimination.
The role of multiple doses of activated charcoal as gastrointestinal dialyzer is being recognized in the treatment of poisoning, due to drugs. On the other hand, chelating agents like BAL, penicillamine and DMSA form complexes with heavy metals, thereby preventing or reversing the binding of metallic cations to body ligands.
Antidotes counteracting the toxic injury: The agents in this group reverse a chemically induced damage or functional disturbance and restore physiological conditions. Amyl nitrite, sodium nitrite, sodium thiosulphate, methylene blue, dantrolene, benzylpenicillin, glucagon, oximes, etc. are common examples.
In general, antidotes should be given in adequate doses as early as possible in cases of poisoning. Some antidotes cause serious adverse reactions. Hence, both the risk and the benefits of the antidotal therapy must, therefore, be carefully evaluated and the patient must be monitored regularly.
At times the half-life of some antidotes like naloxone, atropine is much shorter than the toxin, in which cases the antidotal therapy must be continued till the symptoms of the poisoning subside.
Disclaimer: This content is information purpose only

| Sr. No. | Chemicals | Antidote/Medical treatment |
| 1. | Acids and Sulphur Oxides (SOx), or Alkalis | a) Wash with plenty of water if the eyes or skin are affected. b) Do not give chemical antidote because it increases heat and injury with reaction. Do not induce vomiting. c) Milk, lemon water or milk of magnesia can be given. |
| 2. | Acetonitrile, Acrylonitrile, Lactronitryl, Cyanogen chloride or bromide | Very careful treatment of cobalt E.D.T.A. (calocynor) and if that is not effective give nitrite/thiosulfate treatment. |
| 3. | Alkali phosphates and Ammonia | Immediately give water or milk and induce vomiting. For the hypocalcemic effect of phosphate give 5 ml intravenous injection of 10% calcium gluconate. If the eye or skin is affected wash with plenty of water for 15 min. |
| 4. | Ammonia | If the skin is affected then wash with plenty of water for 15 min. and then wash with dilute lactic acid and apply soframycin cream. If the eye is affected then wash by eye fountain with plenty of water for 15 min. Put one drop of 0.4% Benzocaine (Novocaine) solution in the eye. Boric or lactic acid solution eye drops can also be given, If entered in the throat then give smell through cotton dipped in ethanol or ether through the nose. Administer oxygen in case of breathing difficulty. |
| 5. | Aniline, Toluidine, and Nitrobenzene | Methylene- Blue (1% solution). Ascorbic acid (5% solution) Administer oxygen in case of breathing difficulty. |
| 6. | Anticoagulants (Heparin) etc. | Protamin sulphate (1% solution), Vitamin-K (1% solution). |
| 7. | Antimony and Stibine | Dymer caprol (BAL) |
| 8. | Arsenic | BAL (British Anti Lewistic compound) ie Dimercaprol, penicillamine. Induce vomiting. |
| 9. | Arsine (Hydrogen arsenide) | Mercaptide (40% solution, Dimercaptopropanol, penicillamine)./ |
| 10. | Atropine | Pilocarpine (1% solution). Proserin (0.05% solution). |
| 11. | Barium and it’s salt | Magnesium sulfate (30 gm in 250 ml water). Morphine (5 to 10 mg.) |
| 12. | Barbiturates | Barmegride (0.5 % solution). |
| 13. | Benzene, Toluene & Xylene | Skin is affected then wash with plenty of water. Administer Oxygen or shift to fresh air. Diazepam 0.1 mg / kg. (iv), bed rest. |
| 14. | Beryllium | Calcium edentate, Prednisolone. |
| 15. | Bis-chloromethyl ether | N-acetyl-L-cysteine. |
| 16. | Bleaching solution | Milk, melted ice-cream, eggs, milk of magnesia, aluminum hydroxide gel. Do not give acid antidotes. |
| 17. | Bromides | Skin is affected then wash with plenty of water. Give 1 gm. Salt in water by mouth. If this is not possible then intravenous (iv) injection of normal saline. Give milk and water. |
| 18. | Boric acid and Boron derivatives | Ipecac solution and activated charcoal. Infra muscular (1m) injection of 5% dextrose if nausea. |
| 19. | Cadmium | Calcium disodium edetate i.e. CaNa2EDTA by intravenous or muscle. |
| 20. | Carbon monoxide | Administer Oxygen (100% pure), intravenous injection of 1 gm/kg of 20%mannitol, or 1 mg./ kg of Prednisolone. |
| 21. | Carbon tetrachloride or Chloroform | N-acetyl-L-cysteine. |
| 22. | Carbonyls | Tablets of Sodium diethyldithiocarbamate, 2 tablets immediately and then 1 tablet every two days for the next two days. Administer Oxygen in case of breathing difficulty. |
| 23. | Cardiac Glycosides | Potassium chloride (0.5% solution). Atropine sulphate (0.1% solution), Tefacin calcium (10% solution). |
| 24. | Chlorine, Bromine, Phosgene | Skin is affected then wash with plenty of water. Apply Sodium bicarbonate and again wash with water. The eye is affected then flush eye in eye fountain. Put 2-3 drops in eye of Pontocaine 0.5% solution of Benzocaine (Novocain) 0.4% solution. If inhaled then give smell through ethanol or ether dipped cotton. Give milk, buttermilk or lemon water. Give 02 in case of breathing difficulty |
| 25. | Chlorates | Ipecac solution, activated charcoal, milk. Don’t give Methylene blue. Add 2 to 5 gms. Sodium thiosulphate in 200 ml of 5% Sodium bicarbonate solution and give by mouth. |
| 26. | Cosmetics (Bromates) | Intravenous injection of 1 ml./kg Sodium thiosulphate (10% solution) |
| 27. | Chromium | Dimercaprol. .Give high vitamins, protein and carbohydrates in food. Methylene blue. |
| 28. | Cyanides and Thiocyanate insecticides | Methylene blue or Calocyanides injection. If inhaled gives smell of amyl nitrate ampule (0.2 ml) every 5 minutes. Intravenous injection of Sodium nitrite (3% solution) and Sodium thiosulphate (25% solution) but if blood pressure decreases, then stop it. 4 DMAP (Dimethyl amino phenol) 3 mg/kg, iv, along with thiosulphate. Hydroxocobalamine, 4 gm,iv, in 5% dextrose. Dicobalt edetate, 300 – 600 mp-, iv, over 1-5min. |
| 29. | DDT (Halogenated insecticides) | Ipecac syrup, activated charcoal. Saline cathartic, Diazepam (10 mg.) by intravenous injection, wash skin with soap and water. In case of breathing difficulty administer Oxygen |
| 30. | Dichlorophenoxy acetic acid insecticides | Ipecac syrup, activated charcoal. Saline cathartic, Lidocane (50-100 mg by intravenous injection).. |
| 31. | Dimethyl sulfate | Skin is affected then apply Magnesium oxide paste and give an injection of Corticosteroid. |
| 32. | Dichloro methane | Hydrocortisone (200 mg every 4 hours). In the case of aspiration pneumonia give antibiotics. |
| 33. | Dinitrophenol or Cresols | 5% Glucose saline by intravenous injection. |
| 34. | Ethanol | 2 gm. Of Sodium bicarbonate in 250 ml water, Diazepam 10 mg., by intravenous. Skin or eye is affected then wash with plenty of water. |
| 35. | Ethylene or Diethylene glycol | Ethanol, Calcium gluconate Pyridoxine |
| 36. | Fluorine, Hydrogen fluoride and derivatives. | Intravenous injection of 10 ml. Calcium gluconate (10% solution). If serum magnesium level is low then give 10 ml Milk of magnesia every hour. Give more milk and liquids. If the eye is affected then wash with plenty of water. |
| 37. | Formaldehyde | Milk, activated charcoal or water. |
| 38. | Formalin | Ammonium chloride or Ammonium carbonate (3% solution). |
| 39. | Hydrogen sulphide, other sulphides and Mercaptans | Shift in fresh air or administer Oxygen. Give inhalation of ethanol or ether drops. Amyl nitrite or Sodium nitrite, Pyridoxine 20 mg./kg. or 10% urea 1 gm./kg by intravenous injection. |
| 40. | Hydrogen cyanide | Give inhalation of 0.2 ml amyl nitrite dipped cotton. Sodium nitrite (1% solution). Sodium thiosulphate (30% solution), Cromosmon (1% methylene blue in 25 % glucose solution). |
| 41. | Iodine and compositions | Milk, Fine starch solution, 100 ml of 1% Sodium gluconate 10% solution. |
| 42. | Iron salts | Careful treatment of deferroxamine therapy. |
| 43. | Lead compounds | CaNa2EDTA, D-Penicilliamine (oral), BAL (with CaEDTA), Induce vomiting, then give Magnesium sulphate in water. |
| 44. | Magnesium salts | Intravenous injection of 1 ml/ kg of Calcium gluconate 10% solution. |
| 45. | Manganese | Calcium edentate |
| 46. | Mercury as Hg, Alkyl or Aryl compounds | Give white of egg in water. Later give milk, Then induce vomiting. BAL, D-Pencilliamine, n-Acetylcysteine, Dimercaptopropane- 1 sulfonate DMPS). |
| 47. | Metals (Heavy metals, mercury, lead, copper, cobalt, arsenic, nickel) | Unithol (BAL, dimercaprol, 5% solution), Tetacin calcium (10% solution), Penicillamine Dextrose (10%) by intravenous injection. Chillating agent for effect of mercury. |
| 48. | Metal Compounds (Heavy metals compositions) | Activated carbon (carbolin) BAL. |
| 49. | Methanol | Ethanol (30% solution from inside, 5% solution from outside i.e. by intravenous injection), Epicake Syrup. In the case of acidosis give Sodium bicarbonate. In the case of delirium give Diazepam 10 mg. by intravenous injection. Folinic acid (Leucovorin), 1 mg/kg, iv, 4 hourly. |
| 50. | Metaldehyde | D-Penicillamine, Ascorbic acid or Thiamine to be given carefully. |
| 51. | Naphthalene | 5 gm. Sodium bicarbonate every 4 hrs. and keep urine alkaline. Give 1 ml/kg, furosemide in liquid. Blood transfusion till haemoglobin becomes normal -60 to 80%. |
| 52. | Nitrates, Nitrites, Nitrobennzene Sulfonamides Dapsone | Methylene blue, 1-2 mg / kg, iv, over 5 min. |
| 53. | Nitrogen oxides (NOx) | Prednison or prednisolone 5 mg. every 6 hrs. interval. |
| 54. | Organic phosphate or carbamate insecticides (abet, diazinon, dimate, EPN, Ethyl Phosphamidon, Phosvel, Selithion, Aldecarb, Baygon, Sevin etc.) | Ipecac syrup, Atropine sulphate 2 mg. by intravenous injection every 3-8 mins interval. Prelidoxim by intravenous. Obidoxim (Toxogonin), skin to be washed with soap and water. |
| 55. | Orgao phosphorous insecticides (e.g. Malathion, Parathion, Monocrotophos, Phorate) | Atropine injection, atropine sulphate (0.1% solution), Nalorphine hydrochloride (0.5% solution), Trimedoxim bromide (15% solution), Pyridine Aldoxy Methyodate, Diperoxim, Biodexim and Isonitrocin (40% solution), Pralidoxim, RAM, TOXOGONIN. |
| 56. | Oxalic acid | Milk, lemon water, chalk or calcium lactate, calcium chloride or calcium gluconate with liquid. 10% calcium gluconate or chloride 10 ml. by intravenous injection. |
| 57. | p-Nitro Chlorobenzene (PNCB) | Methylene blue |
| 58. | Phenol & Derivatives | Shift in fresh air, activated charcoal and 240 ml. milk. If skin or eye is affected then wash with plenty of water for 15 min. If skin is affected then wash with Polyethylene glycol(PEG). |
| 59. | Phosgene | Cortisone acetate 1 mg./kg by mouth – thrice a day. In case of breathing difficulty administer Oxygen |
| 60. | Phosphorous, Phosphine & Phosphides | 10 ml. Calcium gluconate (10%) by intravenous injection, 5% glucose in water. Travert (10% invert sugar) by intravenous injection. |
| 61. | Potassium permanganate | Hot milk, Methylene blue (1% solution) Ascorbic acid (5% solution) |
| 62. | Silica & Asbestos dust | Reduce dust level by local exhaust ventilation. Use airline respirator. |
| 63. | Silver nitrate & other salts | 10% Salt (Sodium chloride) solution, milk and for reducing, pain Demrol or Codeine. |
| 64. | Tobacco & Nicotine | Induce vomiting, Atropine (large dose). In case of difficulty in breathing, administer Oxygen. |
| 65. | Vinyl chloride | Skin is affected, wash with plenty of water. Eye is affected then keep eye open and allow material to vaporise. Don’t apply any eye drops In case of breathing difficulty, administer Oxygen. If injected then induce vomiting. Give one spoon mineral oil and after that give sodium/magnesium sulphate (one spoon) in a glass of water. Give strong tea or coffee if feeling exhausted. |
| 66. | Zinf fumes and metal fume fever | Prednisolone, Aspirin, Bed rest. |
NOW ITS YOUR TURN / अब आपकी बारी
PLEASE SHARE THIS ARTICLE WITH YOUR RELEVANT FRIENDS
शेयर करें



good Awareness
Good morning Mr. Saurabh
My name is Suresh Kumar working as HSE Manager in Qatar. All your works are great and much useful in my profession.
Thank you for the great job done and may God Bless You… Stay well
Excellent